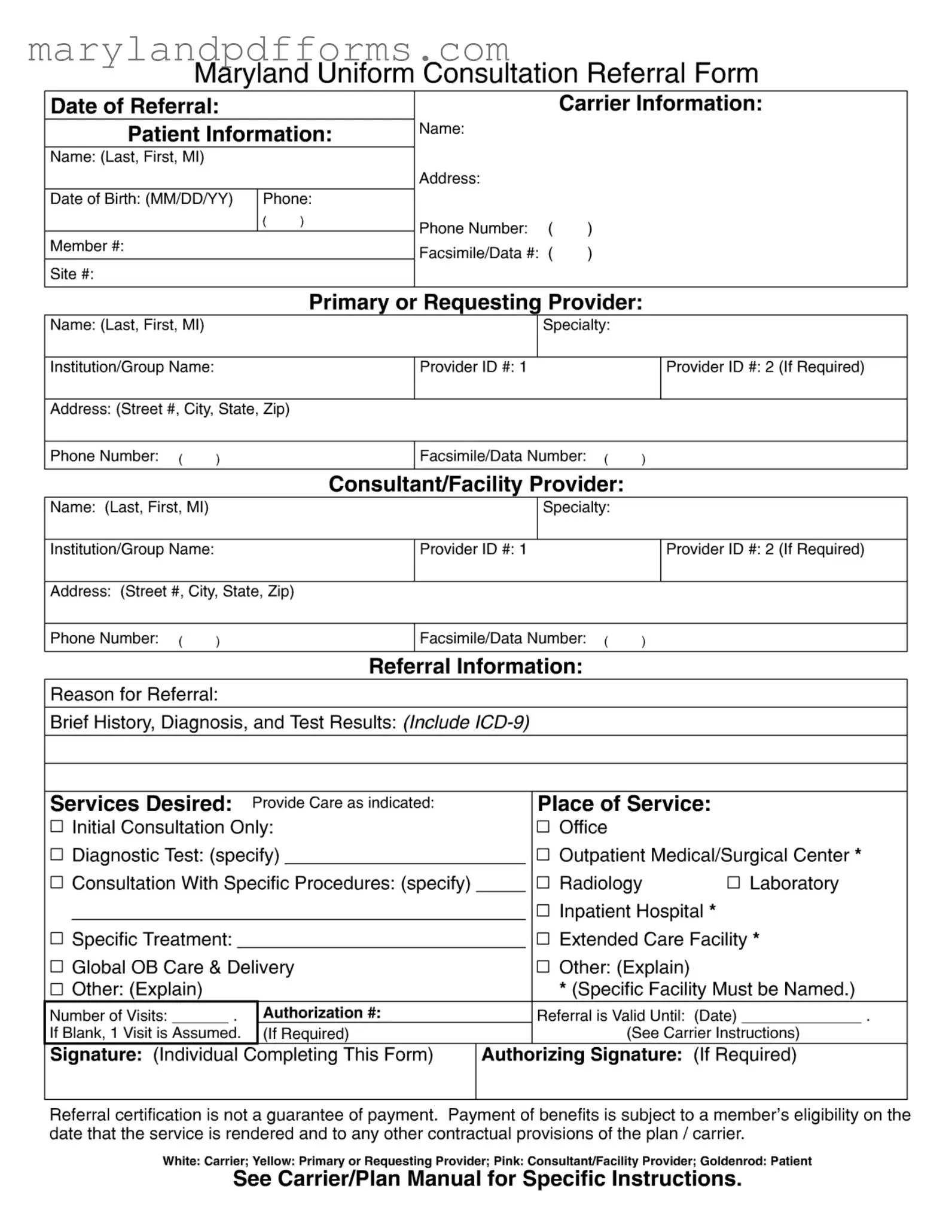
Blank Maryland Referral Template
Similar forms
The Maryland Referral Form shares similarities with several other documents commonly used in healthcare and insurance processes. Here are six documents that are comparable:
- Consultation Request Form: This document requests a specialist's evaluation for a patient. Like the Maryland Referral Form, it includes patient information, provider details, and the reason for the consultation.
- Marital Separation Agreement: To navigate the complexities of separation, refer to our essential Marital Separation Agreement resources for guidance on legal documentation and obligations.
- Prior Authorization Request: This form seeks approval from an insurance carrier before specific services are rendered. It requires patient and provider information, as well as details about the requested services, similar to the referral process.
- Patient Intake Form: Used at the beginning of a patient’s visit, this form gathers essential information such as demographics and medical history. It parallels the Maryland Referral Form in collecting patient data and contact information.
- Transfer of Care Form: This document is used when a patient is transferred from one provider to another. It shares the need for detailed patient information and the reason for the transfer, akin to the referral form's purpose.
- Authorization for Release of Medical Information: This form allows healthcare providers to share patient information with other entities. It includes patient consent and provider details, similar to the referral form's requirements for authorization.
- Insurance Claim Form: This document is submitted to an insurance company to request payment for services rendered. It requires patient and provider information and details about the services, much like the Maryland Referral Form.
Maryland Referral - Usage Steps
Once you have the Maryland Referral form in hand, it's time to fill it out carefully. Each section requires specific information to ensure that the referral process goes smoothly. After completing the form, it will be submitted to the appropriate parties for processing. Follow these steps to fill out the form accurately.
- Date of Referral: Write the date when you are completing the form.
- Carrier Information: Fill in the relevant details about the insurance carrier.
- Patient Information: Enter the patient's name (last, first, middle initial), date of birth (MM/DD/YY), phone number, member number, and site number.
- Primary or Requesting Provider: Provide the name, specialty, institution/group name, and provider ID number for the primary provider. Include their address and phone number.
- Consultant/Facility Provider: Fill in the name, specialty, institution/group name, and provider ID number for the consultant or facility. Also, include their address and phone number.
- Reason for Referral: Clearly state the reason for the referral.
- Referral Information: Provide a brief history, diagnosis, and test results, including the ICD-9 codes.
- Services Desired: Indicate the services required, such as initial consultation, diagnostic tests, or specific treatments.
- Place of Service: Select the appropriate place of service, like an office, outpatient center, or inpatient hospital. Specify if necessary.
- Number of Visits: Indicate the number of visits if applicable. If left blank, one visit is assumed.
- Authorization Number: Fill in this section if required.
- Referral Valid Until: Write the expiration date for the referral.
- Signature: Sign the form to indicate completion.
- Authorizing Signature: Include this if required for the referral.
Once the form is filled out, review it for accuracy before submitting it. Keep a copy for your records, as it may be needed for future reference. Remember, completing this form does not guarantee payment; it is essential to ensure that the patient is eligible for coverage on the date of service.
Learn More on Maryland Referral
What is the Maryland Referral Form used for?
The Maryland Referral Form is a document used by healthcare providers to refer patients to specialists or other facilities for additional care. It ensures that all necessary information is communicated clearly, helping to facilitate the patient's treatment process. The form captures essential details about the patient, the referring provider, and the consultant or facility provider, streamlining the referral process.
What information do I need to provide on the form?
When filling out the Maryland Referral Form, you will need to provide the following information:
- Date of referral
- Carrier information
- Patient information, including name, date of birth, and contact details
- Primary or requesting provider details, such as name, specialty, and provider ID
- Consultant or facility provider information
- Reason for referral and any relevant medical history
- Services desired and place of service
- Authorization details, if required
Completing all sections accurately helps ensure the referral is processed smoothly.
Who should complete the Maryland Referral Form?
The form should be completed by the primary or requesting provider who is referring the patient. This provider is responsible for ensuring that all necessary information is included and that the form is submitted to the appropriate consultant or facility provider.
How long is the referral valid?
The referral is valid until the specified date indicated on the form. If no date is provided, it is assumed that the referral is valid for one visit. It is important to check with the carrier’s instructions to understand any specific validity periods that may apply.
What if I do not have an authorization number?
If you do not have an authorization number, you can leave that section blank. In this case, it is assumed that the referral is for one visit. However, it is advisable to confirm with the patient's insurance carrier to ensure that all necessary authorizations are in place for the services being requested.
What should I do if the referral is not approved?
If the referral is not approved, the patient or the referring provider should contact the insurance carrier for clarification. It may be necessary to provide additional information or documentation to support the referral request. Understanding the reasons for denial can help address any issues and improve the chances of approval in the future.
Can I use this form for all types of referrals?
While the Maryland Referral Form is designed for a variety of referrals, it is essential to ensure that it meets the specific requirements of the patient's insurance plan. Some plans may have their own referral forms or additional documentation requirements. Always check the carrier's instructions to confirm compliance.
Is the referral certification a guarantee of payment?
No, referral certification does not guarantee payment. Payment of benefits is contingent upon the member's eligibility on the date services are rendered and any other contractual provisions of the insurance plan. It is crucial for both providers and patients to understand this to avoid unexpected costs.
Additional PDF Forms
Maryland W-4 - Detailed reporting of acquisitions and disposals during the fiscal year is required.
In order to effectively manage and mitigate risks associated with various activities, it's essential to utilize legal instruments such as the Arizona Hold Harmless Agreement, which is readily available through resources like Templates Online. This agreement ensures that one party is protected from potential liability, making it a crucial element for individuals and organizations engaging in activities with inherent risks.
Md Form 502 Instructions - If vouchers for subsequent installments are needed, indicate it on the form.
Documents used along the form
The Maryland Referral Form is an important document used in healthcare to facilitate communication between healthcare providers regarding patient referrals. However, there are several other forms and documents that are often used in conjunction with this referral form to ensure a smooth process. Below is a list of these documents, each described briefly for clarity.
- Patient Intake Form: This form gathers essential information about the patient, including medical history, current medications, and contact details. It helps healthcare providers understand the patient's background and needs before the initial consultation.
- Operating Agreement Form: This form outlines the management structure and operational guidelines of a limited liability company (LLC) in New York, defining the rights and responsibilities of its members. For more details, visit PDF Templates Online.
- Authorization for Release of Information: This document allows healthcare providers to share the patient’s medical records with other providers involved in their care. It is crucial for maintaining continuity of care and ensuring that all providers have access to relevant information.
- Insurance Verification Form: This form is used to confirm the patient's insurance coverage and benefits. It helps providers understand what services are covered under the patient’s plan, ensuring that the referral and subsequent services are authorized for payment.
- Clinical Summary: A clinical summary provides a concise overview of the patient’s medical condition, previous treatments, and any relevant test results. This document is often shared with the consulting provider to give them a clear understanding of the patient’s situation.
- Follow-Up Appointment Scheduling Form: After the referral is made, this form is used to schedule the patient’s follow-up appointments with the consulting provider. It ensures that the patient receives timely care and helps manage their treatment plan effectively.
Utilizing these documents alongside the Maryland Referral Form enhances communication among healthcare providers and supports better patient care. Each form plays a specific role in the referral process, ensuring that all necessary information is exchanged efficiently.
Key takeaways
When filling out the Maryland Referral Form, it's essential to ensure accuracy and completeness. Here are some key takeaways to keep in mind:
- Accurate Patient Information: Always double-check the patient's name, date of birth, and contact details. This information is crucial for proper identification and communication.
- Provider Details: Include accurate information for both the primary/requesting provider and the consultant/facility provider. This ensures seamless coordination of care.
- Reason for Referral: Clearly state the reason for the referral. This helps the consultant understand the patient's needs and the context of the referral.
- Services Desired: Specify the services needed, such as initial consultations or diagnostic tests. Clarity here can streamline the process and avoid misunderstandings.
- Place of Service: Indicate where the services will be provided. This could be an office, outpatient center, or hospital. Specificity is key, as certain facilities may require prior authorization.
- Authorization and Validity: Be aware that a blank authorization field typically assumes one visit. Additionally, note the expiration date of the referral to ensure timely service delivery.
By following these guidelines, you can enhance the efficiency of the referral process and improve patient care outcomes.
Misconceptions
Misconceptions about the Maryland Referral Form can lead to confusion and frustration. Below are seven common misconceptions along with explanations to clarify each one.
- The form guarantees payment for services rendered. Many believe that completing the referral form ensures payment. However, referral certification does not guarantee payment. Payment depends on the member's eligibility and the specific provisions of their plan.
- All fields on the form are optional. Some individuals think they can leave sections blank. In reality, certain fields, such as patient information and reason for referral, are essential for processing the referral correctly.
- The referral is valid indefinitely. There is a misconception that referrals do not expire. Each referral has a validity period, which must be noted on the form. If this date is left blank, only one visit is assumed to be authorized.
- Any provider can be listed as a consultant. Some may assume that they can refer to any provider. However, it is crucial to ensure that the consultant is within the member’s plan network to avoid unexpected costs.
- Referral forms are the same across all carriers. Many think that the referral process is uniform. In truth, different carriers may have specific instructions and requirements. Always check the carrier's manual for guidance.
- Only primary care providers can submit referrals. There is a belief that only primary care providers can complete the form. In fact, any authorized provider can fill out the referral form, as long as they have the necessary information.
- The form does not require a signature. Some individuals might think that a signature is not necessary. However, the form must be signed by the individual completing it, and an authorizing signature may also be required for certain referrals.
Understanding these misconceptions can help ensure a smoother referral process and better communication between patients, providers, and carriers.